Carotid Angiography
What is carotid artery disease?
Like the blood vessels of the heart (coronary arteries), the carotid arteries also develop atherosclerosis, the build-up of fat and cholesterol deposits, called plaque, on the inside of the arteries. Over time, the build-up narrows the artery, decreases blood flow to the brain and can lead to a stroke.
What is carotid angiography?
Carotid angiography, also called carotid angio or an arteriogram, is an invasive x-ray imaging procedure used to detect the presence of narrowing or blockage (atherosclerosis) in the carotid arteries.
Carotid angiography may be performed when carotid artery disease is suspected, based on the results of other tests, such as a carotid duplex ultrasound, computed tomography angiogram (CTA) or magnetic resonance angiogram (MRA)..
What is carotid angioplasty and stenting?
Carotid angioplasty is a non-surgical procedure performed after the diagnostic angiogram. The carotid angioplasty procedure can be performed the same day as the diagnostic angiogram or days or weeks after the angiogram.
 During angioplasty, a balloon catheter is guided to the area of the blockage or narrowing. When the balloon is inflated, the fatty plaque or blockage is compressed against the artery walls to improve blood flow.
During angioplasty, a balloon catheter is guided to the area of the blockage or narrowing. When the balloon is inflated, the fatty plaque or blockage is compressed against the artery walls to improve blood flow.
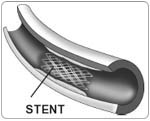
During the angioplasty procedure, a carotid stent (a small, metal mesh tube) is placed inside the carotid artery at the site of the blockage and provides support to keep the artery open.
For patients who meet certain eligibility criteria, carotid stenting offers a less invasive approach than carotid endarterectomy, the traditional surgical treatment for carotid artery blockages. During carotid endarterectomy, an incision is made in the neck at the site of the carotid artery blockage. The artery is isolated and the plaque and diseased portions of the artery are surgically removed. Then, the artery is sewn back together to improve blood flow to the brain. In contrast, carotid stenting can be performed while the patient is awake, reducing recovery time and the risk of complications and re-narrowing.
What happens during the carotid angiography procedure?
A medication such as heparin may be given during the procedure to reduce the risk of blood clots. You may also need to take aspirin and/or Plavix (clopidogrel bisulfate) for 3 to 5 days before the procedure and for 4 to 6 weeks after the procedure. Your doctor or nurse will give you specific instructions. First, the doctor anesthetizes or numbs the area where the introducer sheath will be inserted. The sheath is a thin, hollow tube that is inserted through a small puncture and into an artery in the leg (femoral approach) or arm (brachial approach).
A long, narrow tube called a catheter is inserted through the sheath and is guided through the aorta to the carotid artery with the aid of a special x-ray machine.
Some patients may have a second sheath placed in the leg or arm vein where a temporary pacemaker wire is placed in the heart to regulate the heart rhythm during the procedure.
Contrast material is injected through the catheter and x-ray movies are created as the contrast material moves through the carotid arteries. The digital photographs of the contrast material are used to identify the site of the narrowing or blockage.
An additional imaging procedure, called intravascular ultrasound (IVUS), may be performed along with carotid angiography in some cases to obtain detailed images of the walls of the blood vessels. IVUS is currently only available in specialized hospitals and research centers. A miniature sound-probe (transducer) is positioned on the tip of the catheter. The catheter is threaded through the carotid artery and, using high-frequency sound waves, produces detailed images of the inside walls of the arteries. IVUS produces an accurate picture of the location and extent of plaque.
If the diagnostic tests show severe narrowing or a blockage in the carotid artery, the carotid angioplasty and stenting procedure may be performed to open the artery, or surgery may be recommended.
What happens during the carotid angioplasty and stenting procedure?
A specially designed guide wire with a filter is placed beyond the site of the narrowing or blockage in the carotid artery. Once the filter is in place, a small balloon catheter is guided to the area of the blockage. When the balloon is inflated, the fatty plaque or blockage is compressed against the artery walls and the diameter of the blood vessel is widened (dilated) to increase blood flow. The balloon is removed and the stent is placed inside the artery to widen the opening and support the artery wall.
After the stent is placed, an angiogram is performed to confirm that the stent has completely expanded and the narrowing or blockage has been corrected. Often, a second balloon catheter is inflated to ensure the stent is maximally opened. The stent stays in place permanently and acts as a scaffold to support the artery and keep it open. After several weeks, the artery heals around the stent.
In clinical trials at Cleveland Clinic, several types of carotid stents have been used along with a device called the embolic protection device (EPD). The EPD looks like an umbrella or wind sock and contains a basket to catch plaque particles dislodged during the stenting procedure. Catching these particles prevents them from traveling in the blood to the brain and reduces the risk of a blood clot or stroke.
How long has the carotid stenting procedure been performed?
The stenting procedure has been performed in clinical trials at Cleveland Clinic since the procedure was introduced in 1994 as an investigational treatment for carotid artery disease.
In 2004, the carotid stenting procedure was approved by the FDA as a treatment option for select patients who have carotid artery stenosis and meet certain criteria. The procedure is approved for patients who are experiencing symptoms, have a carotid artery that is blocked 70 percent or more, and for whom surgery would be highly risky.
Research is still ongoing to compare the results of the carotid stenting procedure with that of the carotid endarterectomy surgery. In a 2005 systematic review of five randomized trials comparing the two treatment options, there were no significant differences in major risks of the two treatments. However, the reviewers concluded more research is needed before carotid stenting can be recommended as the treatment of choice for suitable patients with carotid artery stenosis.
Common Questions About the Carotid Stenting Procedure
How can I find out if I am eligible for the procedure?
If the carotid stenting procedure is recommended as a treatment option, you will be evaluated to determine if you meet the eligibility requirement for this procedure. Some carotid stenting procedures are performed as research procedures. You may also ask your doctor if you meet the criteria to participate in a research protocol or clinical trial.
If you are an eligible candidate for the carotid angioplasty and stenting procedure, your doctor and nurse will give you more information about what to expect before, during and after the procedure.
Will I be awake during the procedure?
Yes. You will awake and conscious during the entire procedure. The doctor will use a local anesthetic to numb the catheter insertion site.
How long does the procedure last?
The procedure usually lasts about 2 hours, but the preparation and recovery time add several hours. Please plan to stay at the Cleveland Clinic all day for the procedure, and remain in the hospital overnight.
What are the risks of the procedure?
Your doctor will discuss the specific risks and potential benefits of the procedure with you. The risks vary, depending on the severity of your disease, location of the blockage, whether you've had a previous stroke and the presence of other medical conditions.
Some of the possible risks include:
- Allergic reaction to the medication or contrast material used during the procedure
- Irregular heart rhythm
- Bleeding at the catheter insertion site
- Stroke or death
There may be other possible risks. When you meet with your doctor, please ask questions to make sure you understand why the procedure is recommended and what the potential risks are.
What happens after the carotid stenting procedure?
The sheath remains in place until the doctor determines when it can be removed, usually a few hours after the procedure. Because nausea can occur while the sheath is in place, you will be limited to drinking clear liquids until the sheath is removed.
You will be required to lay flat (without bending your legs) after the sheath is removed. This is necessary to prevent bleeding. You may receive medication to reduce discomfort. Your doctor will determine how long you will have to lay flat, which could be from 2 to 8 hours. To close the wound where the sheath was placed, you may have either a collagen seal or stitch placed in the artery, OR pressure will be applied to the site.
Plan on staying overnight in the hospital after the procedure. You will be evaluated by your doctor, have a neurological exam, and have other tests, such as a carotid ultrasound, to evaluate the results of the procedure. Your doctor will discuss the results of the procedure with you and your family.
Before you go home, you will be given instructions about your medications, diet, activity, and when to call your doctor. You will need to monitor your blood pressure when you go home, so your doctor or nurse will teach you how to take and record your blood pressure. You will need to buy a home blood pressure monitoring system to accurately record your blood pressure.
Your doctor will prescribe aspirin and Plavix (clopidogrel bisulfate) to take for a few months after the procedure. These medications help prevent blood clots from forming at the site where the stent was placed. Follow your doctor's instructions about how and when to take these medications. Do not stop taking these medications without first talking to your doctor.
You will need to take it easy for a few days after the procedure. You may climb stairs, but use a slower pace. Do not strain during bowel movements.
Gradually increase your activities until you reach your normal activity level by the end of the week.
What is restenosis?
Restenosis is a return of a blockage or a re-narrowing in the treated carotid artery. It is more likely to occur in the first 6 to 12 months after treatment, so keeping your follow-up appointments is important. Restenosis is caused by the accumulation of scar tissue at the treatment site. The rate of restenosis, as reported in current clinical research, is 1 percent per year.
If you have symptoms similar to what you experienced before the procedure, call your doctor as soon as the symptoms occur.
Does the carotid stenting procedure cure carotid disease?
For most people, the carotid angioplasty and stenting procedure increases blood flow to the brain and decreases the risk of a stroke.
Although the carotid stenting procedure opens up a blocked carotid artery, it does not CURE carotid artery disease. You will still need to focus on reducing your risk factors and making certain lifestyle changes to prevent future disease development or progression.
To achieve the best results, you must be committed to living a healthy lifestyle that includes quitting smoking, taking medications as prescribed, taking and recording your blood pressure, following a heart-healthy diet, managing high blood pressure, cholesterol and diabetes and following up as recommended with your health care team.
Advanced Reproductive Technology
- In Vitro Fertilisation (IVF)
- Intracytoplasmic Sperm Injection (ICSI)
- Donor egg and embryo programs
- In Vitro Fertilisation (IVF)
- Pre-implantation genetic diagnosis (PGD)
- Surrogacy programs
Dental Videos