|
Intrauterine Insemination (IUI)
Introduction Intrauterine insemination or IUI is a basic step towards fertility treatments. It is also called artificial insemination. This fertility treatment can be done using your husband or partner's sperm or sperm from a donor. An intruterine insemination is a very low tech form of fertility treatment. It is generally used in two ways: natural and with ovulation induction. 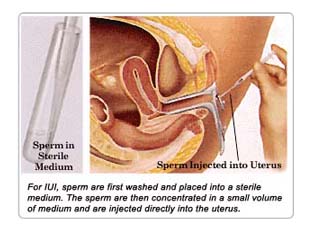
In a natural cycle, you will monitor your body for ovulation. When you detect an LH surge you will be instructed to contact the fertility clinic for further instructions. They will tell you when and how to collect a sperm sample. Depending on the fertility clinic you may be required to collect the sperm sample in the office. What is an IUI and how is it done? An IUI intrauterine insemination is performed by threading a very thin flexible catheter through the cervix and injecting washed sperm directly into the uterus. The whole process doesn't take very long it usually only requires the insertion of a speculum and then the catheter, a process that maybe takes a couple of minutes (60-90 seconds to introduce the catheter, then sperm injection, and another 60 seconds or so to remove the catheter going slowly helps reduce discomfort). Sometimes when the cervix is hard to reach a tenaculum is used to hold the cervix, which makes the process a bit more uncomfortable.
Where is the sperm collected? How long before the IUI? Usually the sample is collected through ejaculation into a sterile collection cup, but it is also possible to obtain collection condoms for this purpose (through the doctor's office Milex is one company that makes them). Most clinics want the semen to be delivered within a half hour of ejaculation, around the time of liquefaction, so if one lives close enough the sample can be collected at home. If not, one has to make do with a room at the clinic, a bathroom, or any private setting. There is a delay between when the semen sample is dropped off for washing and when it is inseminated. The amount of time depends on the washing technique used, which takes 30 minutes to two hours, as well as on the clinic's scheduling. Most will perform the IUI as soon after washing is completed as possible. When is the best timing for an IUI? Ideally an IUI should be performed within 6 hours either side of ovulation for male factor infertility some doctors believe after ovulation is better, otherwise chances of success are higher with insemination before ovulation with the sperm waiting for the egg. When timing is based on an hCG injection, the IUIs are usually done between 24 and 48 hours later. Typical timing would be to have a single IUI at about 36 hours post-hCG, though some do it at 24 hours, and some clinics are reporting better results when doing the IUI at 40-42 hours post-hCG. If two IUIs are scheduled, they are usually spaced at least 12 hours apart between 24 and 48 hours after the hCG. Some reports show no increase in success rates with two IUIs, but others suggest it may increase success as much as 6 percent. Some doctors will base timing of IUI on a natural LH surge. In that case, a single IUI at 36 hours is the norm, but doing them at 24 hours is also pretty common since ovulation may be a bit earlier. When two inseminations are planned, they are usually timed between 12 and 48 hours after the surge is detected. The egg is only viable for a maximum of 24 hours after it is released. CandidatesIUI is usually recommended for couples with no known cause of infertility who have been trying to have a baby for at least one year. You should have a thorough infertility investigation before trying IUI. Under normal circumstances, IUI uses sperm from the male partner. However; another insemination technique, artificial insemination by donor (AID) or therapeutic donor insemination (TDI), uses screened sperm samples from anonymous donors. Reproductive Science Center adheres to the guidelines of the American Society for Reproductive Medicine regarding the use of donor sperm. It is the ASRM's position that under present circumstances, the use of fresh semen for donor insemination is not warranted. All frozen specimens should be quarantined for 180 days and the donor should be retested and found to be seronegative for HIV before the specimen is released. This position is consistent with our goal to provide safety for patients undergoing this procedure. Male partner requirements - IUI relies on the natural ability of sperm to fertilize an egg within the reproductive tract. Studies show that IUI will not be effective in cases where the male has low sperm counts or poor sperm shape. Sperm tests should show reasonable sperm function:
Female partner requirements - The female partner should have no obvious fertility problems. Tests should show normal ovulation, open fallopian tubes, and a normal uterine cavity.
Benefits The success rates of superovulation (from hormone treatment) and IUI are between 5 and 15 percent per cycle (dependent on the woman's age) provided that the male partner's sperm count is within normal limits and the female's tubes are healthy. Doctors might try three cycles of IUI and, if these are not successful, then recommend more advanced methods such as in vitro fertilization (IVF). Unlike IVF, IUI does not involve egg collection or general anesthetic. Risks While complications of IUI are infrequent, they can include infection, brief uterine cramping, or transmission of venereal disease (from donor semen). Risks of the hormone treatment for controlled ovarian hyperstimulation include multiple pregnancy and Ovarian Hyperstimulation Syndrome (large ovaries and collection of fluid in the abdomen). If more than three follicles mature, there is a risk of multiple pregnancy. Your doctor may choose to stop the treatment cycle. Multiple pregnancies tend to have higher rates of miscarriage, lower birth-weight babies, and greater social difficulties. Your doctor may also stop the cycle if you have Ovarian Hyperstimulation Syndrome, a rare effect. Too high a dose of drug can cause excessive stimulation of the ovaries, which you may notice as pain in the abdomen. Procedure
Advanced Reproductive Technology FREE QUOTE PATIENT SPEAK ‟We had almost lost hope and given up. But we are thankful to God, for blessing us with our little angel. Today we have a reason to smile and celebrate. We would also like to thank Paradigm for all the help and support. ‟We are so happy. After several failed attempts my wife finally got pregnant. She is 10+ weeks pregnant now. Eagerly awaiting the arrival of our baby. ‟After 10 years of marriage we have finally been blessed with a girl child. All credit to the doctors and the staff. ‟Thanks a lot for helping us achieve our goal of starting a family. We feel very fortunate to have been under your care and able guidance for our treatment. We really appreciate the kind of service and care that you provided us. |